Unstable Transitions in HVAC Operations: Operating Room Occupancy Modes
Miles Ryan, P.E., writes a monthly column in Engineered Systems Magazine on Building Commissioning. Read October’s column below:
Periods of instability in HVAC system operations often occur during necessary transitions in system operation. Examples of such instances include when a system first enables, goes from occupied to an unoccupied mode of operation, or key components of the system (chillers, pumps, etc.) stage on or off to meet system demands.
Additional provisions in the automation of these systems are required to minimize the effects of these disturbances. Determining the exact provisions needed is often delegated to the temperature controls contractor. Design documents often include blanket statements such as “it is responsibility of the temperature controls contractor to implement rate limiters, time delays, and/or deadbands, as well as further refine setpoints and control loop tuning parameters to promote stable system operation.” That statement is intentionally vague and all encompassing, the designers do not want to start prescriptively detailing every step the temperature controls programmer needs to take. They expect the temperature controls contractor to understand design intent of the sequence and fill in the blanks on how to achieve that intent in a stable manner.
Typically, not all the kinks are worked out prior to the functional performance testing directed by the commissioning provider. Our testing processes should be paying extra close attention during the transitional periods to identify any levels of unexpected instability, and we should also have a solid understanding of the tools available to the temperature controls contractor to improve performance in such instances. This column, as well as next month’s, details examples of unstable transitions that can occur and how they can be addressed.
Operating Rooms: Occupied vs Unoccupied Modes
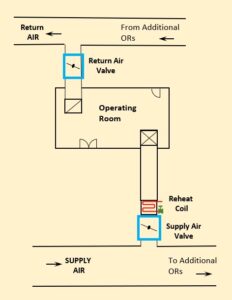
Figure 1: Operating Room Diagram.
Note: Locations and quantity of supply air diffuser and return grille shown are not actual, rather they are shown diagrammatic purposes.
Operating rooms are very energy intensive spaces. They require high air changes per hour (ACH), tight temperature and humidity tolerances, and need to consistently remain positively pressurized in relation to adjacent spaces. The high amounts of supply air coming from the serving AHU at a typically low supply air temperature (~48°F), drives up cooling energy consumed by the AHUs, as well as fan energy. There is also substantial energy consumed at the supply air valve’s reheat coil as to prevent the spaces from being overcooled. A common energy saving opportunity specified by design engineers is to have an Unoccupied Mode programmed for the space. The space can enter the Unoccupied Mode of operation, which will reduce the supply airflow into the space to save energy, when either of the following scenarios are encountered:
- The space is scheduled unoccupied on the BAS. For example, from 6 PM to 6 AM.
- The space is scheduled to be Occupied, but the occupancy sensors in the space have not detected movement for a period of time (e.g. 30 minutes).
The space will need to remain positively pressurized in all scenarios though. Therefore, as the supply airflow is reduced in Unoccupied Mode, the return airflow is also reduced as to always be sucking less airflow out of the space than what is being supplied to it.1
On a recent project, prior to testing, we could see through trend review (Figure 2) that the operating room was correctly reducing its supply airflow (and in turn the ACH) during the scheduled unoccupied period (the first of two scenarios which would index the space into Unoccupied Mode). Initial review of the trends seemed to indicate occupants entered periodically enough throughout the day that that space never really went into Unoccupied Mode during the scheduled occupied period. However, during functional performance testing, instability in the transition from Occupied Mode operation to Unoccupied Mode operation was identified when trying to verify the system enters Unoccupied Mode in the second scenario listed above.
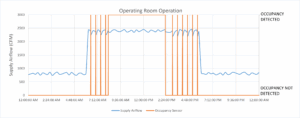
Figure 2: Trend of operating room supply airflow and occupancy sensor.
The system was operating in Occupied Mode, then we exited the space so the occupancy sensor would stop detecting our presence. Once the time delay was realized after the occupancy sensor stopped triggering, the supply airflow setpoint reduced from roughly 2,400 CFM to 800 CFM, and the supply air valve quickly throttled airflow. The return valve tracks on an offset below measured supply airflow, so there is a delay in how quickly that return valve can respond. This delay in return air valve operation resulted in a brief period of negative space pressure. This negative pressure pulled the inswing door open, which triggered the occupancy sensor, which put the room right back into Occupied Mode! Closer review of the trend data (Figure 2) confirmed the unit never remained in Unoccupied Mode when scheduled occupied. It wasn’t people in and out of the space that kept the occupancy sensor occasionally triggering, it was the system attempting to enter Unoccupied Mode, and the resultant door swinging inward, that was triggering the occupancy sensor. Trend data showed the occupancy sensor momentarily triggers on 30 minute intervals. Without being present just outside the operating room during functional performance testing, this scenario may never have been caught, and the hospital would have paid the excess energy costs for many years to come.
The Fix
The solution to maintain a positive pressure in the operating room while transitioning from Occupied Mode into Unoccupied Mode, and in turn prevent the unstable triggering of the occupancy sensor, was to put a rate limiter on the active supply airflow setpoint for the space. Essentially, the effective supply airflow setpoint would slowly drop from occupied setpoint (2,400 CFM) to unoccupied setpoint (800 CFM) over the course of 10 minutes. This allows the return valve to respond quick enough to the slow drop in measured supply airflow and prevent pulling a negative pressure in the space. Such a rate limiter when going from Unoccupied Mode (800 CFM supply air setpoint) to Occupied Mode (2,400 CFM supply air setpoint) was not needed. An instantaneous step change in setpoint was tested. The magnitude of the space’s positive pressure went slightly higher than the design team was targeting, but not large enough to prevent staff from entering the space. It was deemed acceptable given the real-world scenarios that would force the space to enter Occupied Mode. We would not want to be slowly walking up the ACH in the space while a surgical team is rushing a patient in for an impromptu surgery, so a rate limiter on how fast the supply airflow setpoint could increase was omitted.
Conclusion
Commissioning providers need to pay extra attention to major operational transitions when testing HVAC systems. That is where instability often occurs. Post additional members of the team either on different computers to review multiple items on the BAS simultaneously, or physically locate additional personnel throughout the building when necessary as to allow for all areas of concern to be reviewed simultaneously. It is relatively easy to get a system to run well in one mode or another, it is much more difficult getting it to transition between modes stably.
References:
1 Ryan, M. 2023. “Adding Resiliency to Pressure Control of Critical Spaces.” Engineered Systems Magazine (Dec).